Introduction
Obesity is a global health problem, with rates nearly tripling in the past 45 years. Non-Alcoholic Fatty Liver (NAFL), excessive fat storage in the liver, affects 50-70% of obese individuals and increases the risk of type 2 diabetes. A healthy diet is crucial in obesity and NAFL management. Both low-carbohydrate and low-fat diets effectively reduce liver fat in overweight individuals.
The quality, rather than just the percentage, of dietary fat and carbohydrates is important. Saturated fatty acids (SFA) increase liver fat compared to polyunsaturated fatty acids (PUFA). Similarly, high-glycemic index (GI) diets contribute to liver fat accumulation. However, previous studies were conducted under unrealistic conditions and did not reflect typical dietary patterns.
The researchers aimed to investigate whether individuals could reduce liver fat content by improving their diet within realistic settings. Comparing a low-GI/SFA diet to a high-GI/SFA diet, they aimed to assess the impact of lowering GI and SFA intake while maintaining macronutrient composition.
Understanding the underlying pathways involved in liver fat modulation is essential. SFA reduces whole-body fat oxidation and increases ectopic fat accumulation. High-GI diets promote glycogen storage and de novo lipogenesis while reducing fat oxidation. Simultaneously reducing SFA and GI may be a viable strategy to manipulate hepatic fat content.
Goal of the study
The study investigated whether a two-week low-GI/SFA diet, compared to an isocaloric high-GI/SFA diet, reduces liver fat content in overweight individuals. Additionally, they examined changes in whole-body fat oxidation, glycemic response, hepatic glycogen levels, de novo lipogenesis, and saturated hepatic fat fraction.
These findings contribute to understanding the impact of dietary interventions and the associated metabolic pathways, aiding the development of improved strategies for managing obesity and complications like NAFL.
Methods used
Thirteen participants were enrolled in a randomized crossover trial, where they followed each diet for two weeks with a washout period in between. The impact of the diets was assessed through various measurements, including respiration chamber measurements.
During the respiration chamber measurement, participants stayed in a controlled environment where their oxygen consumption, carbon dioxide production, respiratory exchange ratio, fat oxidation, and carbohydrate oxidation were continuously measured. The participants received meals matching their assigned diet during the overnight stay in the chamber. The sleeping metabolic rate and substrate oxidation were evaluated.
The respiration chamber measurements provided valuable insights into the participants’ energy expenditure, respiratory exchange ratio, and substrate utilization. These measurements helped determine the metabolic effects of the low-GI/low-SFA and high-GI/high-SFA diets, shedding light on how these dietary patterns influence whole-body energy metabolism and fuel utilization.
By utilizing the respiration chamber, the researchers were able to gain a comprehensive understanding of the metabolic responses associated with the different diets. This information contributes to our knowledge of how dietary interventions, specifically focusing on GI and SFA content, can impact energy expenditure and substrate oxidation, ultimately influencing liver fat content and metabolic health in overweight individuals.
Results
Participants closely adhered to the prescribed diets, as confirmed by food checklists and weekly checkups. Although body weight slightly decreased in both diet groups during the first week, there were no significant differences in body weight changes between the two diets.
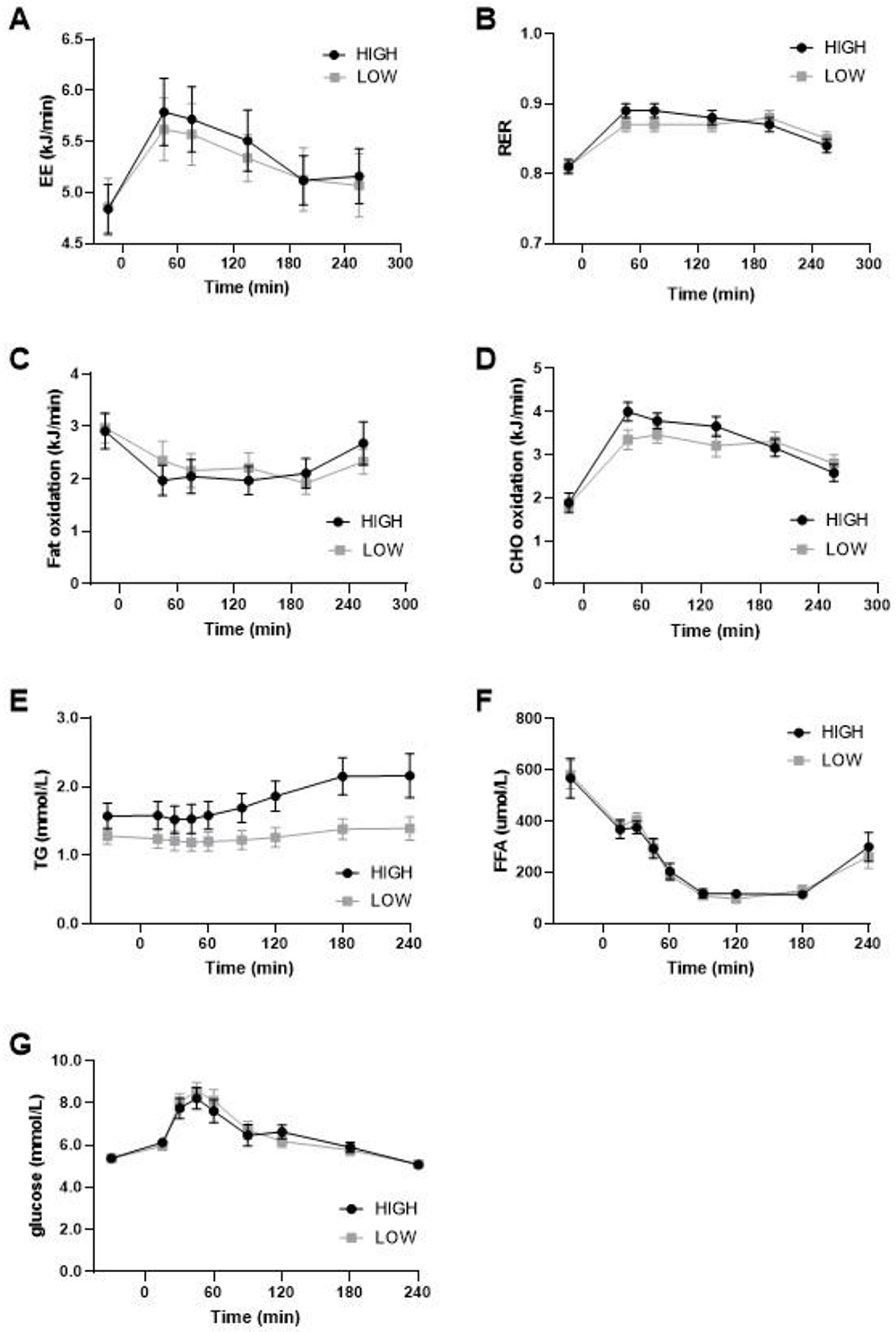
Notably, the measurement of energy expenditure provided valuable insights. Sleeping metabolic rate, carbohydrate oxidation, and fat oxidation during sleep did not significantly differ between the low-GI/SFA and high-GI/SFA diets. Furthermore, the respiratory exchange ratio and substrate oxidation were similar under fasting conditions and after a breakfast meal. Total energy expenditure did not significantly differ between the diets.
In terms of glycemic response, the low-GI/SFA diet demonstrated lower glycemic variability and lower glucose levels after lunch compared to the high-GI/SFA diet. However, no significant differences were observed in hepatic glycogen content or hepatic de novo lipogenesis between the two diets.
Regarding plasma markers, triglyceride levels were significantly lower in the low-GI/SFA diet both in the fasted state and throughout the meal test, while there were no significant differences in plasma glucose and free fatty acid levels.
Overall, these results suggest that while the low-GI/SFA diet did not significantly affect energy expenditure or body weight compared to the high-GI/SFA diet, it exhibited favorable effects on glycemic response and plasma triglyceride levels. These findings contribute to our understanding of the metabolic effects of different dietary patterns in overweight individuals.
This figure depicts the results of a meal test conducted after a two-week period of either a high- or low-glycemic index/saturated fatty acid (GI/SFA) diet. (A) Energy expenditure (EE) during the meal test did not differ significantly between the two diets. (B) The respiratory exchange ratio (RER), indicating substrate utilization, was similar for both diets. (C) Fat oxidation and (D) carbohydrate oxidation during the meal test showed no significant differences between the high- and low-GI/SFA diets. (E) Plasma triglyceride levels exhibited a significant effect of diet and diet × time interaction. (F) Plasma-free fatty acid levels and (G) plasma glucose levels did not differ significantly between the diets. These findings suggest that the high- and low-GI/SFA diets had differential effects on plasma triglyceride levels, while not significantly impacting energy expenditure, substrate oxidation, or plasma glucose and free fatty acid levels during the meal test.
Conclusion
This study aimed to investigate the impact of dietary macronutrient quality, specifically glycemic index (GI) of carbohydrates and saturated fatty acid (SFA) content, on liver fat storage and metabolic parameters. The findings revealed that a two-week isocaloric low-GI/low-SFA diet, compared to a high-GI/high-SFA diet, resulted in a reduction in liver fat content and improved glycemic response. However, there were no significant differences observed in hepatic glycogen, hepatic de novo lipogenesis, whole-body substrate oxidation, or total energy expenditure between the two diets.
The results align with previous research demonstrating that dietary macronutrient quality plays a crucial role in modulating liver fat content. Notably, the low-GI/low-SFA diet led to a substantial 28% decrease in intrahepatic lipid (IHL) content compared to the high-GI/high-SFA diet. Moreover, individuals initially classified with non-alcoholic fatty liver (NAFL) based on their IHL content following the high-GI/high-SFA diet no longer met the criteria for NAFL after switching to the low-GI/low-SFA diet. These improvements were achieved within a short two-week period, emphasizing the significance of macronutrient quality in liver health.
Regarding metabolism, the study found no significant differences in hepatic glycogen, hepatic de novo lipogenesis, or whole-body substrate oxidation between the two diets. Additionally, there were no substantial variations in total energy expenditure. These findings suggest that the effects of dietary macronutrient quality on liver fat content and glycemic response may not be primarily mediated through changes in these metabolic processes.
While the study focused on indirect calorimetry and energy expenditure, further research is warranted to explore the specific mechanisms underlying the reductions in liver fat. Other pathways involved in liver fat accumulation, such as FFA uptake, dietary fat storage, and VLDL-TG secretion, should also be considered in future investigations.
In conclusion, this study underscores the significance of macronutrient quality in reducing liver fat content and improving glycemic response. Adopting dietary patterns that minimize GI and limit SFA intake can yield substantial benefits for liver health. However, the effects on liver fat content and glycemic response observed in this study may not be directly linked to changes in hepatic glycogen, hepatic de novo lipogenesis, whole-body substrate oxidation, or total energy expenditure. Further studies are needed to unravel the precise mechanisms involved and to explore additional metabolic pathways associated with different dietary patterns.
Related products
Whole body room calorimeters
The Room Calorimeter, used in numerous research studies, is spotlighted for its unparalleled accuracy and reproducibility in measuring energy expenditure in various contexts. This tool is vital for generating reliable data in studies exploring energy expenditure during various activities, from 24-hour energy expenditure evaluations to high-intensity exercise testing.
How can we help you with your research?
Maastricht Instruments creates equipment in the field for indirect calorimetry measurements. We provide support for studies, research and measurements alongside our indirect calorimetry products. Consult us about our indirect calorimetry metabolic cart, whole room calorimeter systems or accelerometry add-ons. Please contact us or find more information on our information pages.
Article reference
Basset-Sagarminaga, J.; Roumans, K.H.M.; Havekes, B.; Mensink, R.P.; Peters, H.P.F.; Zock, P.L.; Mutsert, R.d.; Borén, J.; Lindeboom, L.; Schrauwen, P.; Schrauwen-Hinderling, V.B. Replacing Foods with a High-Glycemic Index and High in Saturated Fat by Alternatives with a Low Glycemic Index and Low Saturated Fat Reduces Hepatic Fat, Even in Isocaloric and Macronutrient Matched Conditions. Nutrients 2023, 15, 735. https://doi.org/10.3390/nu15030735